Autistic people have told the care regulator about the “undignified and inhumane” care they have been subjected to in mental health units, including the frequent and traumatising use of segregation and restraint in England.
They spoke to the Care Quality Commission (CQC) as part of its government-commissioned review into the use of restraint, seclusion and segregation for autistic people and people with learning difficulties and mental health conditions.
In the report, Out of Sight – Who Cares?, CQC says it found “too many examples of undignified and inhumane care, in hospital and care settings where people were seen not as individuals but as a condition or a collection of negative behaviours”.
The response to this was often to “restrain, seclude or segregate them”.
The review calls for “fundamental change in the way care is planned, funded, delivered and monitored”, so it is “underpinned by a firm foundation of human rights”, and restraint, seclusion and segregation “are no longer accepted and are only used in extreme cases”.
Many of those subject to restraint described to CQC its “lasting and traumatising effects”, with one saying: “I feel absolutely f***ing sh*t about being restrained.
“It makes me feel …dehumanised. I don’t feel like a real human being.”
Another said: “It feels like my freedom has been taken away and I am powerless.”
One of the autistic people the review spoke to – Alexis – described how she sought help from mental health services because of a lack of appropriate community care.
During an initial 72-hour admission to hospital, she experienced a “catastrophic clash” between her autism and the lighting, noise and chaos of the “box” she was kept in, and quickly became “overloaded”.
In the following months, she was restrained 97 times and secluded 17 times, was forcibly drugged, and her body was left “battered and bruised”, and her identity “fractured”.
She told the review: “They didn’t like the autistic part of me. I tried to tell them that autism is all of me, it’s who I am.
“I argued that my autism couldn’t be treated. They said I lacked insight.”
After three-and-a-half years, she was eventually able to flee to Africa where she created a new routine and set up an autism-friendly home, weaned herself off the drugs she was taking, received private treatment from a psychologist, and, after six weeks, started to work as a teacher again.
The key to success, she told the review, “is creating the right environment and treating psychological differences with dignity and respect”.
The review found that 81 per cent of 313 wards for children and young people, people with learning difficulties and autistic people, had used physical restraint in the last month.
The review also found widespread use of medicines as “chemical restraint” to control people’s behaviour.
It found so-called “rapid tranquilisation” used in a third of wards for children and young people and people with learning difficulties and autistic people in the previous month, even though the practice has “significant side effects and should only be used as a last resort”.
The review looked in detail at 66 people who were subject to prolonged seclusion (which tends to be shorter-term) or long-term segregation (used to isolate someone away from the main ward for a longer period).
Out of those 66, the review found evidence that just three people received “consistently good quality care and treatment”.
Some of the people it came across had spent up to 13 years in long-term segregation.
Almost 71 per cent of people whose care was reviewed had been segregated or secluded for three months or longer, and some people had been in hospital for more than 25 years, although it was not clear whether they had been in segregation or seclusion for even longer than 13 years.
Most of the people CQC saw were autistic or had learning difficulties, although some had a diagnosis of mental distress.
Overall, the review concludes, people in community-based services were experiencing a better quality of life than those with “comparable complex needs” in hospital settings, and were subject to less restraint.
And many people ended up in hospital because they did not receive the support they needed in the community, the review found.
The review calls for a system of national oversight of people living in adult social care services in the community who are being subjected to “highly restrictive environments”.
Of the people seen by CQC during its review, 60 per cent had been prevented from securing a discharge from a hospital because of a lack of suitable care in the community.
The review makes 17 recommendations for improvements, including a demand that the commission itself improves its regulatory approach, such as increasing the number of unannounced and evening and weekend inspections.
It also says that disabled service-users, their families and advocates must be involved in the development of services and care plans.
The review concludes: “Immediate action is needed to put an end to the abuses in human rights that we have seen throughout this review.
“This action must be owned and led from the top by government, delivered by local systems working together, and involve people and their families to ensure the needs of the individual are met.”
The review also commissioned a group of “experts by experience” – three parents of autistic people and an autistic person, who also acted as the review’s expert advisory group – to analyse the conclusions of previous reports dating back more than a decade on health and social care for autistic people and people with learning difficulties.
They found that their meetings throughout the review with disabled people, parents, carers, chief executives, psychiatrists and others “almost unanimously came up with the same ideas and themes as those identified in previous reports”.
They found a repeated failure to implement the recommendations of previous reports, which was caused by the failure of governments to ensure “adequate, fit-for-purpose” administration, funding, accountability and inspection.
They concluded: “The lack of upfront community funding seems to be the key contributory factor to the failure on the part of all involved to deliver reform.”
But they also criticised CQC for its inspection regime.
They said: “People with a learning disability and autistic people need CQC to implement an inspection framework that is fit for purpose, one that is focused on upholding people’s rights.
“Without this, human rights abuses… will not only continue, but also be inevitable.”
They said that those paid to “police” the system need to find a way to “find, manage and deal with unlawful practice”, adding: “There must be greater oversight and accountability as we presently see the clear consequences of repeated failure to take on board the recommendations of past reports.”
They said that “power must be handed back to individuals (and their families), enabling them to make choices and be the rightful authors of their own destinies.
“If this does not occur, any additional money will be wasted and make little difference to the lives of autistic people, people with a learning disability and/or people with a mental health condition.”
Picture: A Panorama documentary about abuse at the private Whorlton Hall hospital for people with learning difficulties and autistic people caused outrage after it was broadcast in May 2019
A note from the editor:
Please consider making a voluntary financial contribution to support the work of DNS and allow it to continue producing independent, carefully-researched news stories that focus on the lives and rights of disabled people and their user-led organisations.
Please do not contribute if you cannot afford to do so, and please note that DNS is not a charity. It is run and owned by disabled journalist John Pring and has been from its launch in April 2009.
Thank you for anything you can do to support the work of DNS…

 SEND inspections find services in just one in four areas usually lead to ‘positive’ outcomes for disabled children
SEND inspections find services in just one in four areas usually lead to ‘positive’ outcomes for disabled children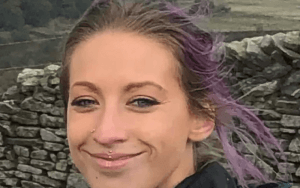 DWP helped cause mental distress of poverty-stricken benefit claimant who took her own life, says coroner
DWP helped cause mental distress of poverty-stricken benefit claimant who took her own life, says coroner Activists will protest over government’s refusal to engage with ‘deep-rooted’ mental health bill concerns
Activists will protest over government’s refusal to engage with ‘deep-rooted’ mental health bill concerns